The 6th Edition of the IDF Diabetes Atlas reports that the number of people living with diabetes rose to 382 million in 2013 and evidence shows that diabetes prevalence by 2035 will be nearly 600 million with diabetes and approximately 470 million will have impaired glucose tolerance. 1 in 8 people in the world, 1 billion people,will live with or be at risk of diabetes.
Bionic Pancreas to Control Blood Glucose
A recently published paper on a study by Boston University and Massachusetts General Hospital provides a boost to the global fight against diabetes. The Bionic Pancreas is a wearable experimental device that has passed the test of constantly monitoring blood glucose and automatically giving insulin or a sugar boosting drug as needed.
The device controls blood glucose in people with Type 1 Diabetes mellitus using doses of both insulin and the blood glucose raising hormone, glucagon.
Unlike other artificial pancreas in the process of being developed that just correct high blood glucose, this one can also fix low blood glucose thereby imitating what a natural pancreas does.
The device has three parts, 2 cell phone sized pumps for insulin and sugar- raising glucagon and an IPhone wired to a Continuous Glucose Monitor. Three small needles go under the skin usually in the belly, to connect patients to the components which can be kept in the pocket.
The study results were published in the New England Journal of Medicine.
New Causes of Neonatal Diabetes
Neonatal diabetes is diagnosed when a child is less than 6 months old and has added complications such as muscle weakness, learning difficulties and, at times, epilepsy.
A study from Exeter (UK) has revealed 2 new genetic causes of neonatal diabetes which affects approximately 1 in 100,000 births and provides further insight into the formation of insulin producing beta cells in the pancreas.
Exeter is a leading centre for neonatal diabetes. Subjects were screened for mutations in genes important for human pancreatic development . Mutations were found which increase the number of known genetic causes of neo natal diabetes to 20.
As well as shedding light on the genetic causes of the disease and providing answers for parents of children with this rare condition, this work helps to understand how the pancreas develops.
Many people with diabetes can no longer make insulin and would benefit from therapies that replace insulin producing beta cells of the pancreas.
(Diabetes Update Spring 2014)
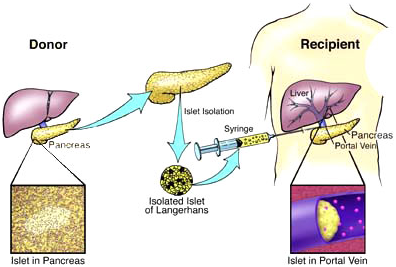
Islet Cell Transplant
The first successful islet cell transplant in the UK took place in 2005. Today it can be a life- saving therapy for those experiencing more than one severe hypo each year.
People who use insulin to control their blood glucose levels sometimes experience episodes of very low glucose or hypoglycaemia.Most people with Type 1 diabetes mellitus are able to manage these hypos because of the characteristic symptoms that tell them when their blood glucose is low such as feeling shaky, sweaty or anxious.
These symptoms are very important because they urge people to manage each hypo thereby preventing their blood glucose levels from falling further which could have potential serious consequences.
Severe hypos can occur in anyone taking insulin but it is more likely to happen in people who have had diabetes for more than 15 years, and thosewho are unable to recognize the low blood glucose level – hypo unawareness.
There are several different medical approaches to help reduce the risk of having a severe hypo.
These include
- The use of multiple injections of modern insulin or
- The use of DAFNE(Dose Adjustment For Normal Eating) style education that help people match their insulin dose to the amount of carbs in each meal.
- Insulin pump therapy sometimes combined with continuous blood glucose monitoring can be helpful.
For people who continue to experience more than one severe hypo each year, an islet celltransplant can be very beneficial and might help them regain control of diabetes. It can be life changing and at times life- saving. They are also suitable for kidney transplant patients who have Type 1 diabetes mellitus and poor blood glucose control.
Islet cell transplantation involves extracting the insulin producing islet cells from the pancreas of a deceased donor and implanting them in the liver of someone with Type 1diabetes mellitus. This minor procedure is usually done twice for each transplant patient and can be performed with minimal risk using a needle under local anaesthestic.
Most people who receive islet cell transplantation continue to take low dose insulin therapy so this is not seen as a cure for diabetes.
Benefits
- Reduces risk of severe hypos
- Leads to improved awareness of hypos
- Less variability in blood glucose levels
- Improved quality of life and reduced fear of hypos.
Risks include a small but increased risk of certain cancers, severe infections and other side effects related to medication needed to prevent the islet cells from being rejected by the body.
The following people might be suitable for an islet transplant:
- Those who have experienced two or more severe hypos within the last two years and have impaired awareness of hypos
- Those with a functioning kidney transplant who experience severe hypos and impaired hypo awareness or poor blood glucose control despite best medical therapy.
The following people are not suitable for an islet transplant:
- Those who need a lot of insulin a day – e.g more than 50 units a day for a 70 kg body weight.
- Who weigh over 85 kg
- Those with poor kidney function.
(balance – May – June 2013)