One of the most commonly occurring complications of diabetes is neuropathy and foot ulcers can occur as a result. Foot ulcers are not easy to recognize or diagnose while they are developing. However, they do show some early warning signs … The place where an ulcer is likely to appear will be a warmer spot on your foot.
A new device uses temperature data to predict whether an ulcer will develop more than a month before it actually shows up. This information is very helpful because it gives more time for doctors to treat it.When doctors aren’t able to treat foot ulcers at an early stage, it can lead to amputations.
Using the device is simple
“People who use it have nothing to do except they have to keep it turned on and step on it each morning,” Doctor of Podiatric Medicine Robert G. Frykberg says. This takes a thermogram of their feet and sends off the data to a central server. A difference of four or more degrees Fahrenheit on two successive days will register an alert, which is then transmitted to the user and to his or her doctor for necessary treatment.
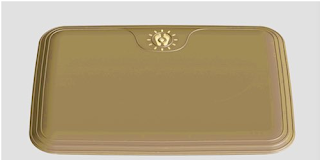
The U.S. Food and Drug Administration approved the marketing of the device in September 2015, and the United States Patent and Trademark Office granted a U.S. patent in February 2016. A start-up company, Podimetrics in Somerville, Massachusetts, makes the device and manages the system. Its Remote Temperature Monitoring System includes the Podimetrics Mat.
A new device uses temperature data to predict whether an ulcer will develop more than a month before it actually shows up. This information is very helpful because it gives more time for doctors to treat it.When doctors aren’t able to treat foot ulcers at an early stage, it can lead to amputations.
Using the device is simple
“People who use it have nothing to do except they have to keep it turned on and step on it each morning,” Doctor of Podiatric Medicine Robert G. Frykberg says. This takes a thermogram of their feet and sends off the data to a central server. A difference of four or more degrees Fahrenheit on two successive days will register an alert, which is then transmitted to the user and to his or her doctor for necessary treatment.
The U.S. Food and Drug Administration approved the marketing of the device in September 2015, and the United States Patent and Trademark Office granted a U.S. patent in February 2016. A start-up company, Podimetrics in Somerville, Massachusetts, makes the device and manages the system. Its Remote Temperature Monitoring System includes the Podimetrics Mat.